Patient Assessment Whats Your Problem Again Ppt
The A-G method is a systematic and structured approach to patient assessment useful both in daily nursing practise and emergency situations. This article provides a stride-by-step description of the method
Abstract
The A-Yard method is a systematic and structured approach of assessing patients, useful both in routine and emergency situations. It is based on the ABCDE approach used when resuscitation may be needed, extended by 2 additional steps. The ability to perform an A-G cess is a fundamental nursing skill, as information technology should exist standard practice non only in critically ill or deteriorating patients, but in all patients receiving care.
Citation: Cathala Ten, Moorley C (2020) Performing an A-M patient cess: a applied footstep-by-footstep guide. Nursing Times [online]; 116: i, 53-55.
Author: Xabi Cathala is lecturer, School of Wellness and Social Intendance/Institute of Vocational Learning; Calvin Moorley is associate professor for nursing enquiry and diversity in care, Schoolhouse of Health and Social Care/Adult Nursing and Midwifery Studies; both at London South Bank Academy.
- This article has been double-bullheaded peer reviewed
- Scroll down to read the article or download a print-friendly PDF hither (if the PDF fails to fully download please try once more using a different browser)
Introduction
Numerous assessments exist in nursing. They are vital tools in day-to-day practice. The A-Yard cess is becoming a unremarkably used tool in principal and secondary intendance settings. It integrates the process mandated for resuscitation and emergency situations. Withal, information technology is too useful for systematic baseline patient assessment and tin can improve patient mortality in hospital (Griffiths et al, 2018).
A-1000 covers: airway, breathing, circulation, inability, exposure, further information (including family and friends) and goals (Benson, 2017). Its systematic approach has been proven constructive in identifying deteriorating patients or those at risk of deterioration (Dean and Bowden, 2017).
Nurses performing the assessment need to explain to the patient what they are going to do and seek their informed consent. Before budgeted the patient, they need to undertake a risk assessment of the environment to determine whether it is safe to undertake the A-Chiliad cess.
This article is based on the Resuscitation Council's arroyo to an A-E assessment (Resuscitation Council UK, 2015) and guidance from Benson (2017) on how to undertake the F and G elements. Using this structured approach can ensure the reliability of the assessment in any situation. An A-G assessment is not merely used in critically ill or deteriorating patients, but should be standard practice for all patients receiving care. It unremarkably takes a few minutes to complete depending on the practitioner'due south feel.
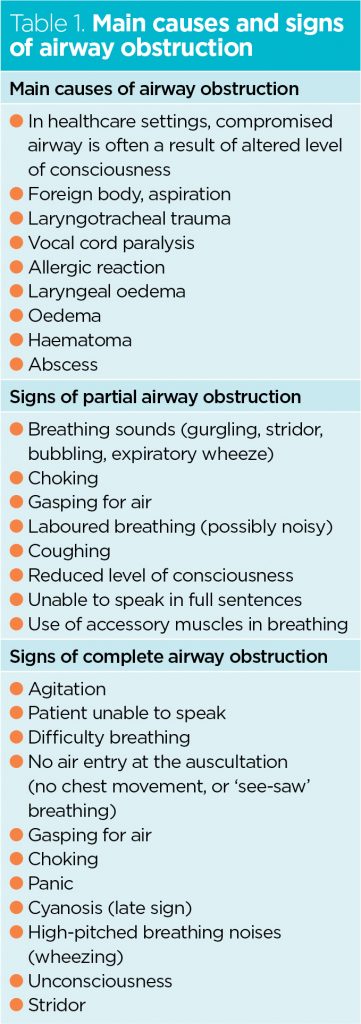
Airway
The airway includes the nose, mouth, larynx, pharynx, trachea, bronchi and bronchioles (Cathala and Costa, 2019). Its main office is to acquit air into the body. The aim of airway assessment is to ensure this anatomical function is achieved and whatever obstacle (total or partial) of the airway is identified (Tabular array ane). An indication of a patent airway is the patient's ability to speak with a usual voice in full sentences.
Breathing
Breathing is the procedure by which air moves in and out of the lungs, allowing gaseous exchange. It should be:
- Effortless;
- Equal bilateral chest expansion;
- At a charge per unit of 12-20 breaths per minute (respiratory rate);
- Noise-free; that is, no wheezing, stridor (a harsh vibrating noise) or rattling;
- The airway should be gratuitous of sputum.
During the assessment, nurses must use the Look, Heed and Feel technique. Looking for any respiratory distress signs (Box 1), assessing the depth and pattern of the respiratory wheel for xv seconds and counting the respiratory charge per unit for a total minute is recommended The acceptable oxygen saturation is >96% for patients without hypercapnic respiratory failure or chronic obstructive pulmonary disease (COPD) and 88-92% for patients with those conditions or at risk of worsening hypercapnia (Williams, 2019; National Guideline Centre, 2010; National Constitute for Health and Care Excellence, 2018; O'Driscoll et al, 2008). The patient's power to talk in full sentences is a good indicator of their breathing status.
Box 1. Respiratory warning signs
- Respiratory distress signs: sweating, key cyanosis, utilize of accessory respiratory muscles (abdominal breathing, 'run across-saw' breathing)
- Respiratory rate <12bpm or >20bpm
- Oxygen saturations outside the normal values, which are:
- >96% for patients without hypercapnic respiratory failure or with chronic obstructive pulmonary disease (COPD)
- 88-92% for patients with hypercapnic respiratory failure or with chronic obstructive pulmonary disease (COPD) or at take chances of worsening hypercapnia
- Breathing noises: rattling, wheezing, stridor, coughing
- Unequal air entry: asymmetrical ascent and autumn of the chest
Listening to the animate sounds tin can give an idea of the cause of any breathing difficulty. Rattling noises can indicate secretion, wheezing tin can infer asthma, while stridor can suggest fractional airway obstruction (Cathala and Costa, 2019).
Placing both hands on the patient's chest to experience for the ascent and fall that accompany breathing will help nurses assess breast expansion and determine symmetry between the correct and left lungs. Consent need to be obtained from the patient and a chaperone should be offered where indicated.
A more accurate assessment is auscultation with stethoscope, but this requires advanced skills.
Apportionment
Assessing circulation is not limited to an assessment of the center. It is focused on the haemodynamic and vascular parts of the circulatory system.
This assessment starts with the peripheries. Are the hands and fingers blueish, pink, stake, warm, cold? Bluish, pale and cold tin reflect a poor peripheral circulation, while pink and warm are linked with a good peripheral circulation.
Another useful measure is capillary refill fourth dimension (CRT). A CRT <2 seconds suggests a good peripheral perfusion (Sansone et al, 2017).
The next part of the cess is the heart rate, taking the peripheral or central pulse. Assessing the pulse involves determining its presence, regularity, quality and volume for 15 seconds. The rate is assessed for 1 full infinitesimal. An acceptable heart rate should exist between 51 and 90 beats per minute (Imperial College of Physicians, 2017). The pulse should be regular and strong or bounding.
An acceptable systolic claret pressure is betwixt 111 and 219 mmHg (Royal College of Physicians, 2017). Clinical readings should exist interpreted with caution. If the systolic blood pressure level differs by ≥10mmHg from the patient's baseline, the effect should be reviewed with some other fellow member of the team. Although diastolic blood force per unit area is non part of the NEWS 2 scoring arrangement a reading it will give a good indication of the patient's haemodynamic status. The estimation of the patient'south fluid input and output should exist calculated using the formula.
It is important to identify signs of haemorrhage, check whether at that place is a bleed present, monitor its output regularly, and ensure the patient has patent intravenous admission, so that fluids tin can exist administered in instance of an emergency (Cathala and Moorley, 2018) (come across Box 2).
Box 2. Cardiovascular warning signs
- Cold, blue peripheries
- Capillary refill time >ii seconds
- Heart rate <51bpm or >90bpm
- Irregular and/or weak pulse
- Systolic blood pressure level <111mmHg or >219mmHg
- Alter in patient consciousness
- Urine output <0.5ml/kg/h
- Signs of haemorrhage
Disability
Disability cess focuses on the main causes of reduced consciousness such as fainting (falls and mobility), drugs (polypharmacy and side effects), booze, poisons and hypoglycaemia. The patient's ACVPU status should be assessed. ACPVU stands for alert, confusion (new), response to vocalization, painful stimuli, and unconscious (Smith et al, 2017).
Other areas of the cess include the pupillary size and reaction to lite: pupils should be of equal size and shape and reactive to low-cal. Nurses also need to cheque the medication chart looking for whatever drug-induced effects.
Measuring blood glucose is an important office of inability assessment. Hypoglycaemia (blood glucose <iv.0mmol/50) can reduce the patient'due south consciousness level (Kitsuta, 2006) and needs to be treated post-obit local trust policies and guidelines. Clinical judgement should be used if the patient is not diabetic; blood glucose levels may not need to be checked simply if there are signs of altered levels of consciousness (Box three) then the claret glucose level should be measured. Measuring arterial or venous blood gas can be helpful in such situations. In diabetic patients with high claret sugar levels, it is of import to expect for signs of ketoacidosis (Box iii).
Box 3. Warning signs of ketoacidosis
- Polyuria (excessive or abnormally large urine output)
- Polydipsia (abnormal thirst)
- Vomiting
- Abdominal pain
- Breath smelling fruity
- Deep or fast breathing
- Very tired or sleepy
- Confusion
- High levels of ketone in blood (>0.6mmol/Fifty) or urine (>2 +)
Pain should exist assessed using a tool such as PQRST (palliate/provoke, quality, radiate, severity/scoring, timing (Falk and Hudson, 2016). A bowel assessment should be undertaken, determining last bowel movement and the quality of the stool using a tool such equally the Bristol stool chart. A medication history, including recreational drugs and alcohol consumption should be taken. Asking for any change in mobility and any falls in the past six months completes the disability assessment.
Exposure
In exposure, nurses will assess the patient for peel rashes, wounds, force per unit area injury, signs of infection, bruises, skin changes (turgor). A tool such as aSSKINg (assessment, pare assessment and skin care, surface, skin, go along, incontinent, nutrition) can exist used (NHS Improvement, 2018). Venous thromboembolism (VTE) assessment should be carried out, using questions such every bit:
- Is the patient at loftier or low risk of VTE?
- Is the patient wearing anti-embolism stockings and/or compression devices?
- Has the patient been prescribed anti-thrombolytic prophylaxis handling?
Nurses must ensure that the patient's dignity and privacy is maintained at all times (including body exposure). In this part of the cess they will examine the patient for signs of pressure injury. Anti-embolism stockings should be removed, every bit pressure injury can exist hidden underneath (NHS Improvement, 2018). Nurses also need to check cannula and drain sites for signs of infection, likewise equally the patient's temperature, which should be between 36.1°C and 38.0°C (Royal College of Physicians, 2017).
A nutritional screening should be undertaken and recorded with a tool such equally the Malnutrition Universal Screening Tool. To consummate this exposure assessment, ostend whatsoever allergies (drugs, medication, food, chemicals) with the patient confronting documentation and think well-nigh which exam(s) and investigation may be relevant.
Further information
F stands for farther data and family and friends. Here nurses demand to gather boosted information from sources such as drug charts, medical notes, investigation results and friends and relatives. A social assessment is needed: who is the patient's next of kin or close relatives? Does the patient live solitary; in a flat or a house? What is admission to the building similar? This will let nurses to develop a picture of the patient'due south surroundings, understand their needs and determine who needs to exist involved in their care. This is specially important for inpatients pending discharge.
Goals
Goals set for the patient will exist based on the results of the cess. The post-obit questions tin be useful:
- What are the goals for the patient (both curt- and long-term)?
- What is the monitoring plan?
It is best exercise to use a SMART (specific, measurable, doable, realistic and timely) arroyo. The practitioner should objectively document patient notes and NEWS charts; and escalate if necessary as per local policies. For handovers, using a structured arroyo such every bit SBAR (situation, background, cess, recommendations) is useful. It is important to reassess patients if their condition changes or as per the monitoring plan put in place.
Box 4. Disability alarm signs
- Change in ACVPU status
- Meaning increment in oxygen requirements
- Modify in pupils' size and/or reaction to lite
- Drug-induced effect afterward dose administration
- Claret sugar <4.0mmol/L
- Hypoxia or hypercapnia
- Change in bowel move
- Presence and/or increasing levels of hurting
- Change in mobility or contempo falls.
ACVPU = Alert, Confusion (new), response to Voice, Painful stimuli, Unconscious
Decision
The ability to perform an A-Chiliad assessment is an important if non mandatory skill. All nurses should be confident and competent in this global systematic practice. Carrying out A-K assessments regularly helps nurses to detect any changes and deterioration and ensure information technology is safe to provide care to the patient. It enables fast action, improving quality of care, patient condom and outcomes. The A-G method could be considered a gold standard assessment.
Key points
- The A-G assessment is a systematic approach useful in routine and emergency situations
- A-G stands for airway, breathing, circulation, disability, exposure, further information and goals
- This offers a systematic approach to patient assessments
- The ability to perform an A-M cess is a key nursing skill
- Re-assessing regularly will help nurses find deterioration early on
References
Benson A (2017) The A-G assessment tool (Airway, Breathing, Circulation, Disability, Exposure, Further information and Goals). Clinical Skills. Net Clinical Skills Express.
Cathala X, Costa A (2019) Beefcake and physiology. In: Moorley C (ed) A Guide to Your First Year in Nursing. London: Sage (in printing).
Cathala X, Moorley C (2018) Selecting intravenous fluids to manage fluid loss in critically sick patients. Nursing Times [online]; 114: 12, 41-44.
Falk KM, Hudson SL (2016) Pain: The 5th Vital Sign.
Griffiths P et al (2018) Nurse staffing levels, missed vital signs and mortality in hospitals: retrospective longitudinal observational study. Health Services and Delivery Enquiry; 6: 38.
Kitsuta Y et al (2006) Changes in level of consciousness and association with hyperglycemia as tool for predicting and preventing re-haemorrhage subsequently spontaneous subarachnoid hemorrhage. Prehospital and Disaster Medicine; 21: 3, 190-195.
National Institute for Health and Intendance Excellence (2018) Chronic obstructive pulmonary affliction in over 16s: diagnosis and management.
NHS Improvement (2018) Pressure Ulcer Core Curriculum. London: NHS Improvement.
O'Driscoll BR et al (2017) BTS guideline for oxygen use in adults in healthcare and emergency settings. Thorax; 72: i1-i90.
Resuscitation Quango Uk (2015) Resuscitation guidelines. The ABCDE arroyo.
Majestic College of Physicians (2017) National Early Warning Score (NEWS) 2.
Sansone CM et al (2017) Relationship between capillary refill time at triage and abnormal clinical condition: a prospective study. Open up Nursing Journal; eleven, 84-90.
Smith GB et al (2017) Vital signs and other observations used to detect deterioration in significant women: an analysis of vital sign charts in consultant-led United kingdom maternity units. International Journal of Obstetric Anesthesia; thirty, 44-51.
Williams B (2019) The National Early Warning Score two (NEWS2) in patients with hypercapnic respiratory failure. Clinical Medicine; 19: 1, 94-95.
Source: https://www.nursingtimes.net/clinical-archive/assessment-skills/performing-an-a-g-patient-assessment-a-step-by-step-guide-06-01-2020/
0 Response to "Patient Assessment Whats Your Problem Again Ppt"
Post a Comment